Cancun Conflicts
14th World Menopause Conference
Long term post-menopausal hormone therapy (HT*) increases the risk of breast cancer, cardiovascular disease and stroke. It reduces fractures and a few other risks, but overall the harms outweigh the benefits so it should not be used for health promotion. For symptoms, “the lowest effective dose should be used for the shortest time” – UK Medicines and Healthcare Products Regulatory Agency (MHRA), or “If you decide to use hormones, use them at the lowest dose that helps. Also use them for the shortest time that you need them” – US Federal Drug Administration.
This good advice doesn’t sell much HT so manufacturers pay “experts” to sit on “advisory boards” and go on “expenses paid” trips to shindigs like this, to say that the FDA and MHRA are wrong, and that HT may actually reduce cardiovascular disease!
Click here for the full programme. The titles suggest many thinly veiled attempts to downplay or throw doubt on the evidence that HT is harmful. In case any speakers forgot to declare their conflicts of interest I’ve listed the publicly available ones.
WHI: An Evolving Understanding of the Clinical Evidence. Speaker Dr Nick Panay.
Dr Panay has received consultancy fees from Pfizer, Bayer, Abbott (click here) plus Baxter, Schering, Eli Lilly, Galen, Janssen Cilag, Merck, Novo Nordisk, Novogen, Organon, Orion, Procter & Gamble, Se-cure, Servier, Shire, Solvay, Storz, and Wyeth (click here).
State of the art HRT. Speaker David Sturdee.
Dr Sturdee has had financial support from Amgen, Theramex, Procter & Gamble, Wyeth, Bayer Schering and Novo Nordisk (click here). In 2010 Athina Tatsioni and her colleagues exposed the 31 biased editorials he has written about HRT (click here).
HRT – Route of administration, dose, age at initiation and duration of therapy. Speaker John Stevenson.
Dr Stevenson has financial conflicts with Schering Plough, Wyeth/Pfizer, Bayer, Meda and Merck/Theramex. I have written about his biased editorials here.
Cardiovascular Effects of Estrogens: Evidence and Hypotheses from Epidemiological Findings. Speaker Rogerio A Lobo
Dr Lobo “has provided consulting services for many large pharmaceutical laboratories” (click here). In 2011 Adriane Fugh-Berman and her colleagues exposed him as a biased editorialist (click here).
Relevance of cardiovascular diseases in menopausal women and their implication for clinical practice. Speaker Dr Peter Collins
Dr Collins served as a consultant to Eli Lilly, Berlex, Merck, Pantarhei, and Pfizer, and has been paid lecture fees by Berlex, Merck, Pfizer, Novo Nordisk, and Organon (click here)
Efficacy and safety of low dose E2/DRSP in postmenopausal women. Speaker Dr David Archer
David F. Archer has consulted for Agile Therapeutics, Bayer Healthcare, Merck, Novo Nordisk, Warner Chilcott, and Wyeth Laboratories (Pfizer), and received honoraria from Bayer Healthcare, Merck, and Wyeth Laboratories (Pfizer) (click here)
Hormone therapy and cardiovascular disease – what is the risk? Speaker John Stevenson (GB)
See above
A cardiovascular guide for menopause physicians – An update. Speaker Peter Collins
See above
BMS Recommendations on Menopause & HRT. Speaker Nick Panay
See above
Strategies to optimize cardiovascular health with HRT. Speaker John Stevenson
See above
What if WHI had just used Transdermal Estradiol and Oral Progesterone instead? Speaker Dr James A Simon
James A Simon has been on the advisory boards of Allergan, Amgen Inc., Ascend Therapeutics, Bayer, BioSante, Boehringer Ingelheim, Concert Pharmaceuticals, Corcept Therapeutics, Inc., Depomed, Inc., GlaxoSmithKline, KV Pharmaceutical Co., Lipocine, Inc., Meditrina Pharmaceuticals, Merck, Merrion Pharmaceuticals, Nanma/Tripharma/Trinity, NDA Partners LLC, Novo Nordisk, Novogyne, Pear Tree Pharmaceuticals, QuatRx Pharmaceuticals, Roche, Schering-Plough, Sciele , Solvay, Teva Pharmaceutical Industries Ltd, Ther-Rx, Warner Chilcott, and Wyeth. Click here.
The optimal new way confirmed by KEEPS. Speaker Nick Panay
See above. Two years after trial completion the KEEPS results have yet to appear in a peer reviewed publication. But they still get presented at conferences to suggest the cardiovascular risks of HT have been overestimated (click here).
Menopausal hormone therapy and osteoporosis: have we completed a full circle? Speaker Tobias De Villiers, conference chair.
Dr de Villiers – has received consultancy fees from Adcock Ingram and Pfizer; speaker’s fees from Servier, and travel support from Amgen, Pfizer, and Bayer (details here)
I don’t know what these speakers said in Cancun. Perhaps they all gave the same good advice as the MHRA and FDA. Perhaps they all paid their own air fares. Perhaps pigs fly.
Jim Thornton
*Hormone replacement therapy (HRT) changed to hormone therapy (HT) Jan 2016
Birth risks
Your birthday was a dangerous day
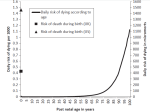
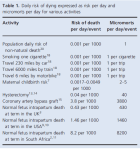
Although the chance of a baby dying during birth in the UK is less than 1 in 2,000 these days, the risk is concentrated in a single day, the day of delivery. My colleagues and I compared that daily risk of 430 per million (430 micromorts) with the chance of dying each day of the rest of our lives. Not until age 92 does the risk per day equal it. Our paper has just been published in BJOG (click here). It will be discussed in BJOG Twitter Journal Club #bluejc on 30 April, and for a week afterwards.
Here is the risk graph, and the main table.
Expressed per day – more dangerous than death row. Half as risky as climbing Everest
I had wanted to compare the risk of birth (430 micromorts) with the daily risk of execution for an inmate of death row in the United States (45 micromorts), or with a day spent above base camp on Everest (820 micromorts) but the BJOG editors dissuaded me. I wonder why!
The point remains. On the day it happens being born is one of the most dangerous things we ever do.
Jim Thornton
Footnotes
Micromorts – David Spiegelhalter has a wonderful site explaining them (click here).
Death row – In 2009, 3,173 inmates spent 1,158,145 days on death row, and 52 were executed (click here), a daily mortality rate by execution of 0.045 deaths per 1000 or 45 micromorts.
Everest – By 2008 there had been 4,102 successful ascents and 216 climbers had died, most in the Khumbu ice fall or at the South Col, both above base camp (click here). If 1 in 4 climbers succeed, each climber has one Sherpa and the average attempt involves eight days above base camp, that equates to 262,528 person days above base camp and a daily mortality of 0.82/1000 or 820 micromorts.
Swiss views
Abolish breast cancer screening
The Swiss Medical Board, an independent group set up by their Ministry of Health to evaluate health technologies, has just reported on mammography screening for breast cancer – full report here, summary in the New Engl J Med (here), or for those without access Abolishing screening.Swiss.
The authors concluded that screening did more harm than good, and that women were being misled. They recommended that no new programmes be introduced, and that time limits be placed on existing ones. Their reasoning was simple.
1. The evidence of benefit comes from rather old trials, and it’s not clear how relevant these are to modern practice. If mammography has improved, the benefit of screening today may be larger than the trials showed, but insofar as conventional treatments of breast cancer have improved, the benefit of screening will be smaller.
2. Any benefit comes at the expense of much harm.
3. The ratio of benefit to harm is hugely overestimated by most women. The authors demonstrated this discrepancy between perception and reality in a simple graphic.
Click on it. It’s worth a thousand words.
Jim Thornton
Bathsheba
Regal misbehaviour
The story, of adultery and murder, is told in the second book of Samuel, Chapter 11. It is spring, the start of the fighting season, and King David’s army is busy destroying the Ammonites and besieging Rabbah. But the King is safely home in Jerusalem, caught up in palace intrigues.
One day, Bathsheba, bathing on the roof of an adjacent house tempts him. He sends for her, one thing leads to another, and soon she is pregnant. This is inconvenient, because she is married to one of David’s best soldiers, Uriah the Hittite, who will be surprised to find his wife pregnant when he eventually returns from the fight. So David sends for Uriah, asks him how the war is going, and tells him to take a day off and go home to visit his wife, hoping thereby to let Bathsheba claim the child is Uriah’s – pregnancy dating was less accurate then. But Uriah doesn’t cooperate. He stays in the palace with David’s servants, and when David remonstrates:
“Camest thou not from thy journey? Why then didst thou not go down unto thine house?”
Uriah replies:
The ark, and Israel, and Judah, abide in tents; and my lord Joab, and the servants of my lord, are encamped in the open fields; shall I then go into mine house, to eat and to drink, and to lie with my wife? As thou livest, and as thy soul liveth, I will not do this thing.”
It’s a fine speech, contrasting the noble Uriah who will not even sleep with his own wife while his men are at war, with David who takes advantage of their absence. David keeps Uriah back from the front for another day and even gets him drunk, but to no avail. He doesn’t go home.
David is ruthless. He writes to his general Joab instructing him to place Uriah at the front where the fighting is fiercest and then to withdraw so Uriah will be killed. To make it worse he gets Uriah himself to carry the message, his own death warrant. The plan works and after a decent period of mourning Bathsheba marries David and bears his son.
But the Lord is displeased. He makes David understand the wickedness of what he has done, and causes the child to fall sick and die. The tough punishment is effective. David learns his lesson, and Bathsheba bears him another son, Solomon, from whose lineage Jesus is eventually born.
But who was really to blame? Can’t kings take mistresses occasionally? Didn’t Bathsheba, a married woman, bathe on the roof where she knew David would see her? The author of Matthew 1: 1-17 refuses even to name her in the list of Jesus’s ancestors. She is simply “her that had been the wife of Uriah”.
Poor practice at BJOG
Hidden sample size change may have altered result
The IRIS trial in this months British Journal of Obstetrics & Gynaecology (BJOG) compared two speeds for administering MgS04 to mothers for fetal neuroprotection. The idea was that the slower one might reduce side effects. The trial report is here. It was registered here. The planned sample size was 140, and the primary outcome any maternal adverse effect. The authors recruited 51 women and found no difference. But they hid their failure to achieve the intended sample by writing, at best incorrectly: “We aimed to recruit 51 women in total.”
Fortunately the editor asked Dwight Rouse, one of the most experienced obstetric triallists in the world, to write a commentary. He checked the trial registration site and picked up the sample size change: “the authors failed to acknowledge it, but should have, the intended sample size when they originally registered the trial was 140 women”.
Good for him. Not good for the editors to fail to make the authors correct the manuscript. Online readers will likely miss Rouse’s commentary.
But it gets worse. The trial registration site now reads “Prospectively registered, target sample size 51, status complete”. Only on the trial registration history here will you find that on 3 March 2013, the sample size was altered from 140 to 51 because “Sample size was based on a reduction in the experience of any adverse effects of the magnesium sulphate infusion (the primary outcome).” This makes no sense. If the rate of the primary endpoint was lower than anticipated, it would be a reason for increasing the sample size!
Does it matter? The results were as follows:
Any adverse event. 15/25 (60%) 60-minute loading; 21/26 (81%) 20-minute loading; risk ratio (RR) 0.74; 95% confidence interval (95% CI) 0.51-1.08. Adverse event leading to ceasing the loading treatment (1/25 in the 60-minute loading group; 2/26 in the 20-minute loading group; RR 0.52; 95% CI 0.05-5.38.
The authors conclusion:
A slower rate of administering the loading dose of magnesium sulphate did not reduce the occurrence of maternal adverse effects overall.
But if the trial had gone on to its planned sample size of 140 and if the percentage of adverse events in each group among the latter 89 had been the same as the first 51 – supposition, but a reasonable supposition – the results might have been 42/70 (60%) v 56/70 (81%). RR 0.74, 95% CI 0.59 – 0.92. P = 0.0078 i.e. slow infusion does reduce side effects.
I know I’m a boring obsessive, but if the question matters, and this one surely does because MgSO4 treatment reduces cerebral palsy, then getting the right answer matters.
This was government funded research. If pharma did this sort of thing, imagine the fuss AllTrials.net would make.
Jim Thornton
Stockholm’s private maternity hospitals
BB Sophia opens
Sweden is far ahead of the UK when it comes to using independent maternity health providers.
Last week a new independent maternity hospital, BB Sophia, (click here) opened in Stockholm. Not a midwife led unit for normal deliveries, or a “too posh to push” place for the super rich to have Caesareans, but a full service maternity hospital, with midwives, obstetricians, anaesthetists and and its own neonatal unit. It will deliver 4,000 babies a year, about the same as the average of the five government-run units in Stockholm. And it’s the second large independent one in the city (click here for the other). They both receive funding per birth from the government, so care remains free to patients.
Compare with the UK. Last year a private midwife unit opened in Cheshire, and the only other one in the country, Tooting in London, closed due to lack of support. And that’s it. The whole of the UK, with a population six times larger than Sweden, doesn’t have a single independent maternity hospital serving NHS patients.
But Sweden is like us in one respect. The usual band of establishment providers are complaining that the new unit will undermine the government ones. The BMA would feel right at home.
Jim Thornton
First FGM Prosecution
What happened?
Female genital mutilation (FGM), the excision all or part of the foreskin/prepuce, clitoris or labia, which causes in some cases labial fusion and narrowing of the vaginal opening, is illegal in the UK.
Campaigners want people who do it, and parents who allow it, to be prosecuted, and last week the director of public prosecutions, Alison Saunders, announced the first one. It’s an odd story. Here is the DPP statement.
“It was alleged that following a patient giving birth in November 2012, a doctor at the Whittington Hospital, in London, repaired FGM that had previously been performed on the patient, allegedly carrying out FGM himself.
“Having carefully considered all the available evidence, I have determined there is sufficient evidence and it would be in the public interest to prosecute Dr Dhanoun Dharmasena for an offence contrary to S1 (1) of the Female Genital Mutilation Act (2003).
“I have also determined that Hasan Mohamed should face one charge of intentionally encouraging an offence of FGM, contrary to section 44(1) of the Serious Crime Act (2007), and a second charge of aiding, abetting, counselling or procuring Dr Dharmasena to commit an offence contrary to S1 (1) of the Female Genital Mutilation Act (2003).”
The newspapers report that Dr Dharmasena had been an obstetrician at the Whittington in 2012 and that Mr Mohamed was related to the alleged victim. What could possibly have happened?
The wording “repaired FGM that had previously been performed on the patient, allegedly carrying out FGM himself” suggests that a midline scar joining the labia across the anterior part of the vagina had torn during the delivery. This is a common post FGM injury. The torn edges bleed so obstetricians are obliged to repair them. They can either place sutures to stop the bleeding but leave the labia separate, i.e return the anatomy more nearly to normal, or they can suture the labia back together across the vaginal opening, i.e. return to the post FGM pre-delivery anatomy.
Although the patient or her partner may request the latter for cultural or sexual reason, it is generally advised against. The delivery has resolved one of the harmful effects of the FGM, and it could be argued that the doctor harms the woman a second time by rejoining the labia. But it’s a stretch to call such a repair FGM. Of course, if the doctor actually removed part or all of a healthy prepuce, clitoris, or labia, that would be FGM, but the DPP’s statement does not imply that.
I dealt with many such cases in the early 1980s when I worked in Africa. My practice was to compromise. I sutured the anterior part of the labia across the vagina but left the posterior part open. I argued that, by leaving a more open vagina, I was making intercourse easier for the woman, but that by repairing the anterior part, I was also respecting the couple’s culture.
It was a more innocent time. I’m glad there were no lawyers looking over my shoulder.
On the face of it this an extraordinary prosecution but perhaps there’s more to it. Ripe-tomato.org will watch the case with interest.
Jim Thornton
Short story
Lydia Davis
A long review of the short story writer in this week’s New Yorker (click here). An early story, The Thirteenth Woman, is two sentences and 138 words long. Not as short as Hemingway’s six word: “For sale: baby shoes, never worn”, but short. Here it is.
The Thirteenth Woman
In a town of twelve women there was a thirteenth. No one admitted she lived there, no mail came for her, no one spoke of her, no one asked after her, no one sold bread to her, no one bought anything from her, no one returned her glance, no one knocked on her door, the rain did not fall on her, the sun never shone on her, the day never dawned for her, the night never fell for her; for her the weeks did not pass, the years did not roll by; her house was unencumbered, her garden unattended, her path not trod upon, her bed not slept in, her food not eaten, her clothes not worn; and in spite of all this she continued to live in the town without resenting what it did to her.
Lydia Davis
Mistakes happen
Glans amputation at neonatal circumcision
Last year ripe-tomato.org drew readers attention to the complications mentioned in a recent WHO manual for teaching neonatal circumcision (click here). Some were serious and probably under-reported; clumsy doctors don’t publicise their mistakes. Parents may sue, but rarely publicise their son’s injury either, and he certainly won’t. We wondered if parents were fully informed.
A recent report (J Paed Urol, Dec 2013, click here, full text here glans amputation) should give cause for thought. Some Canadian urologists describe six cases of accidental amputation, referred over a five or ten* year period. Two were successfully reattached, albeit with deformity; it’s too soon to know whether sensation was affected. The other three required multiple reconstructive operations. Warning – it’s illustrated.
It’s a nice paper. The authors show clearly how the problem happens when the foreskin has not been fully separated before surgery, and how it can be avoided by dividing adhesions between the glans and foreskin. Doctors performing circumcision should read it carefully. Parents will want to ensure their son gets done by an expert – or perhaps leave him intact.
Jim Thornton
* The abstract says the injuries occurred over a five year period, but the main text says over ten. Simple error. Mistakes happen!
A tongue-tie trial
What might it look like
If tongue-tie division improves breast feeding, tens of thousands of babies a year might undergo it in the UK. Sooner or later things would go wrong – scissors would slip, and babies with clotting disorders would bleed heavily. That doesn’t mean we shouldn’t do it. Just that we should be sure it does more good than harm. What might a good quality trial look like?
Pre-trial
Someone with skills in systematic reviewing and no vested interest, should work with the Cochrane Collaboration to pull together the previous trial evidence and decide whether the question has already been answered. Presumably this is in hand.
Funders also need evidence that the association between tongue tie and breast feeding difficulties is real: a study of babies feeding nicely and babies with problems, with tongues all examined by an expert, without knowledge of how the breast feeding is going. If tongue-tie is equally common in both groups we can stop worrying about it. Has there been such a study?
Trial design
The trial must compare division with never dividing. A trial comparing immediate with delayed division has two problems. It precludes measuring any long term outcomes; even duration of breast feeding, let alone anything like speech development or long term health, and it limits participation to staff and parents who already believe it works. Measures of things like nipple pain and breast feeding scores are particularly susceptible to biased reporting, and may be reduced, at least in theory, because the baby is in pain from the division. No-one wants to treat breast pain by hurting the baby.
Would any parent agree to their baby joining such a trial? Many will want one or other option, and recruitment will be a challenge. But many trials have been successfully conducted in other similarly polarised fields. It’ll need many centres, and many parent invitations. No-one would be forced to join.
Some babies in the “no division” group might get divided – it would be impossible and unethical to forbid division forever. To avoid biasing the results in favour of “no division” such babies would be analysed in their original group, by “intention to treat”. But to keep their numbers small, only parents who can give a reasonable commitment to stick with the allocated treatment should join. This will also slow recruitment.
By the time independent randomisation, trial registration, data management, analysis by intention to treat, agreed sample sizes and defined endpoints that don’t get altered are included, the trial might cost £1M or so. But let’s say each division costs £100 and 10,000 babies a year are eligible. If no trial is done the NHS could spend that every year for ever!
If the results are negative the trial would have saved thousands of babies from unnecessary surgery, and the money saved can be spent on other ways to help breast feeding. If division improves breast feeding, it can be rolled out properly, with incalculable health benefits.
Jim Thornton
See also Leave Their Tongues Alone (here) and Another Tongue-Tie Trial (here)